School of Public Health

April 6, 2023
Dr. Shafik Dharamsi joined The University of North Texas Health Science Center at Fort Worth as dean of the school of public health in the fall of 2022. With over 25 years of experience in public health, Dharamsi has committed to preparing the next generation of public health professionals, researchers, and health care leaders…

April 6, 2023
Zhengqi Tan's Work at Pumas-AI in Pharmaceutical Drug Development Zhengqi Tan, Ph.D., MPH, has always been fascinated by the potential of artificial intelligence in solving complex problems. He joined Pumas-AI after completing his Ph.D. in Epidemiology from the HSC School of Public Health in July 2022. Pumas-AI is a company that creates Julia platform-based analytical…
April 4, 2023
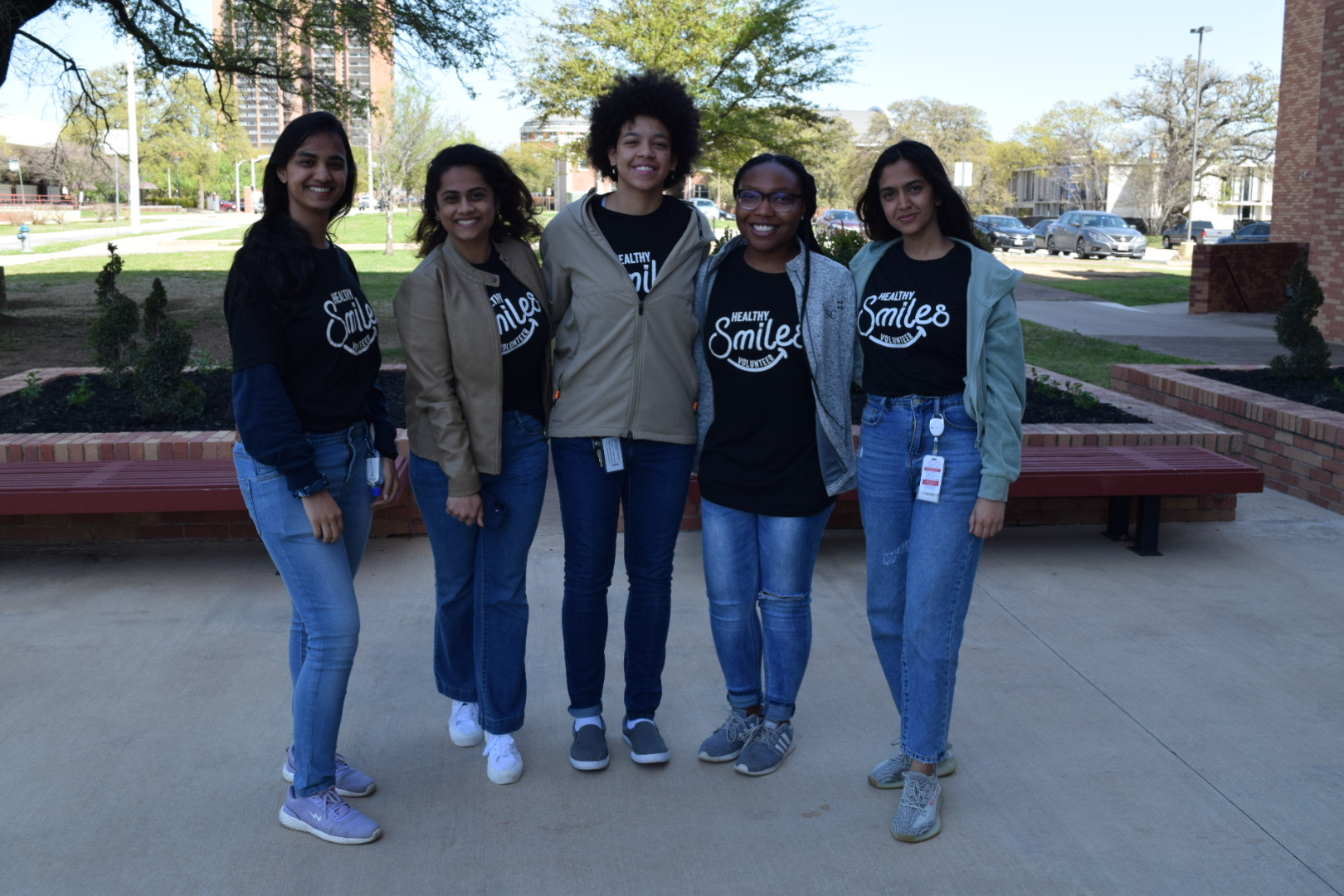
UNTHSC SPH and Texas Woman’s University Dental Hygiene Clinic collaborated to increase HPV Vaccination by educating dental hygienists on recommending the HPV vaccine to prevent oral cancer. Together, they hosted the Healthy Smiles event on March 25th, where children received free preventive dental appointments, vaccine information, and were able to get the HPV onsite. This initiative was supported by…

February 23, 2023
Dr. Eun-Young (E.Y.) Mun, Professor at the University of North Texas Health Science Center (UNTHSC) School of Public Health, has been recognized as a Fellow of the Association for Psychological Science (APS). The APS is a globally recognized organization committed to the advancement of scientific psychology across disciplinary and geographic borders. The APS comprises over…

February 21, 2023
SPH enjoyed hosting the Elevating Power and Black Excellence event to honor Black History Month and celebrate Black Excellence. The panelists discussed uplifting and empowering activities they are doing in our community. Fort Worth Report

December 15, 2022
By Sally Crocker The School of Public Health hosted its second annual Maternal and Child Health (MCH) and Health Disparities Poster Symposium, featuring more than 30 graduate student poster presentations from five courses in the public health core curriculum: Introduction to MCH, Introduction to Health Disparities, Human Sexuality and Reproductive Health, MCH Epidemiology and Epidemiology.…

December 14, 2022
Sally Crocker, Associate Director, Academic Communications, for the HSC School of Public Health, has recently won two new writing awards on behalf of HSC: A Platinum Award from the Association of Marketing and Communication Professionals’ (AMCP) annual, international MarCom Awards competition. MarCom Awards honors excellence in marketing and communication while recognizing the creativity and hard…

December 13, 2022
By Sally Crocker The power of public health was evident at a recent HSC-hosted event to welcome the new Dean of the School of Public Health, Dr. Shafik Dharamsi, and engage with local public health experts to gain their perspectives on building a healthier North Texas community. The highly successful event was well attended and…

Social media