A population at risk
By Jan Jarvis
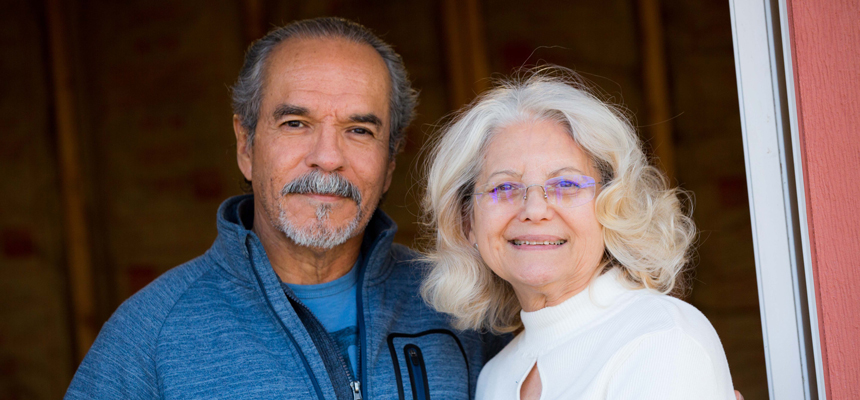
Charles and Teresa Gonzales know what dementia does to a person.
The Grand Prairie couple has lived through it with both of their mothers.
“The first thing I noticed was my mother kept asking the same question over and over,” Charles said. “She’d ask something and a few minutes later, ask it again.”
Teresa Gonzales observed a similar pattern in her mother.
“She would go for a drive and get lost,” she said. “She thought people were stealing from her.”
Charles and Teresa, now part of a comprehensive national study about Mexican-Americans and Alzheimer’s disease, watched helplessly as the mothers they once knew vanished and dementia took over their lives. Their deaths left the couple with lots of questions.
“I wanted to know if I should start preparing for this,” Teresa said. “Should I get my affairs in order before it happens to me? Should I get my Do Not Resuscitate form ready now?”
As much as Teresa wanted answers, her husband did not.
“I just don’t want to know,” he said.
At UNT Health Science Center, they joined one of the largest studies in the United States involving Mexican-Americans and Alzheimer’s disease. One of its goals is to understand why Hispanics develop cognitive loss and Alzheimer’s almost a decade earlier than other ethnic groups.
Teresa hopes to get answers to help her plan for her own future. Charles has a different goal in mind.
“I’m participating so that hopefully this research will lead to a cure someday,” he said. “Yes, go ahead and test me, but even if I’m in the middle of Alzheimer’s, please don’t tell me.”
Tailoring treatment to the patient
Charles and Teresa Gonzales are among the 2,000 volunteers from North Texas needed for the study, including 1,000 Mexican-American and 1,000 non-Hispanic whites. Scientists from the University of Southern California; University of California, San Francisco; and other institutions are collaborating on the project.
The data collected over the five-year study could offer earlier insight into Alzheimer’s and ultimately lead to treatments specifically tailored for Mexican-Americans, said Sid O’Bryant, PhD, Professor, Center for Alzheimer’s & Neurodegenerative Disease Research at UNTHSC.
“This is the first project to specifically attempt to understand how different biological causes relate to Alzheimer’s disease across ethnicities,” Dr. O’Bryant said. “By looking at different potential causes related to memory loss, we may be able to target the right pathway at the right time with the right intervention.”
The ultimate goal: tailoring treatments to a patient’s biology, rather than taking a one-size-fits-all approach to treating Alzheimer’s disease.
The study requires volunteers to undergo an MRI of their brains, as well as blood tests looking for markers for the disease. They also take cognitive skills tests. The results are made available to them.
This study is so extensive that a robot has been purchased to process the 400,000 separate blood tubes that will be stored in a bio-repository at UNTHSC and made available to researchers globally. To handle the 4,000 MRIs required, UNTHSC has contracted with Midtown Medical Imaging in Fort Worth and the Mark and Mary Stevens Neuroimaging and Informatics Institute at the University of Southern California for MRI analyses.
The University of Southern California lab, led by Arthur W. Toga, PhD, is overseeing the storage and analysis of MRI data, including both connectivity maps and structural images. Also participating in the project is Kristin Yaffe, MD, from the University of California, San Francisco’s Weill Institute for Neurosciences.
While her husband has not asked what his results show, Teresa Gonzales has asked that the MRI results be put in her medical records.
“It might be too late for me already, I don’t know,” she said. “But it might help, too.”
The impact
For many volunteers the chance, to make a contribution to science has played a significant role in their decision.
Their participation is indeed important, especially considering the major impact the data can have on Hispanics nationwide.
The number of Hispanics diagnosed with Alzheimer’s disease is expected to grow by more than 800 percent, reaching 1 million by 2030. Yet data about this fast-growing population is extremely limited. Hispanics account for less than 1 percent of participants in clinical trials involving Alzheimer’s disease.
Researchers will use the data to better understand Alzheimer’s. Research suggests that diabetes and depression may be of particular importance in cognitive loss and Alzheimer’s disease among Hispanics.
Hispanics faces a greater risk of developing diabetes than non-Hispanics and are about 50 percent more likely to die from the disease, Dr. O’Bryant said. The same is true for depression, which Hispanics face as much as a 44 percent increased risk of developing than non-Hispanic whites.
“It could be that diabetes and metabolic dysfunction or depression – or perhaps a combination of both – are of major importance to memory loss and Alzheimer’s disease among Mexican-Americans,” he said.
That concerns 63-year-old Jesse Torres, 63, who volunteers five days a week at a community center.
It’s been shown Hispanics develop Alzheimer’s a decade earlier than other ethnicities. Add diabetes and cardiovascular disease to the family profile, and the risk goes up.
“My cholesterol is good, and I don’t have high blood pressure,” he said. “But I have Type 2 diabetes and that scares me.”
He tries to reduce is risk by challenging his mind with dominoes, math games and pool.
“I do a lot of world puzzles because maybe that will lessen the possibility that I will get this disease,” Torres said. “I don’t use a calculator; I just do figures in my head.”
Teresa Gonzales started taking piano lessons and playing Scrabble.
She and her husband also exercise at the gym at least three times a week. Since retiring last March, Charles has been building a shed in his backyard.
Their hope is the study will one day lead to a cure for Alzheimer’s. But until then they’ve come to a truce.
“I know he doesn’t want to know,” Teresa said. “So even if I start seeing symptoms, it is not going to be me who tells him.”
Join the study:
For more information on how to be a study participant, call UNT Health Science Center at 817-735-2963.






Social media