School of Public Health

February 22, 2024
Dr. Malinee Neelamegam, assistant professor of population and community health at The University of North Texas Health Science Center at Fort Worth School of Public Health, has been elected to the executive council of the South Asian Public Health Association (SAPHA). Dr. Neelamegam's appointment to this position reflects her dedication to advancing public health initiatives…

February 16, 2024
By Sally Crocker Dr. Babayemi Olakunde has spent the majority of his career in the coordination of HIV response in Nigeria. The country has one of the highest burdens of HIV/AIDS in the world, with an estimated 1.9 million people living with HIV and nearly 75,000 new infections per year. Nigeria’s mortality rates for women…
February 16, 2024
By Sally Crocker The University of North Texas Health Science Center at Fort Worth recently won a bronze award from the prestigious international Serious Play Conference. The organization honors outstanding digital and board/tabletop games used for training, education or other game-based learning programs. Designed with other HSC collaborators by Emily Belew, MHA, LNFA, instructor in…

February 13, 2024
By Sally Crocker In a unique collaboration, Texas Health Resources has teamed with UNT system schools at both the undergraduate and graduate levels to work collectively on implementing community health projects. The University of North Texas Health Science Center at Fort Worth School of Public Health is one of those partners working with Texas Health’s…

February 13, 2024
By Sally Crocker The School of Public Health at The University of North Texas Health Science Center at Fort Worth has become a member of The Network: Towards Unity For Health, and Dr. Shafik Dharamsi, SPH Dean, has been named to the TUFH international advisory board. TUFH is an official non-state actor of the World…
February 12, 2024
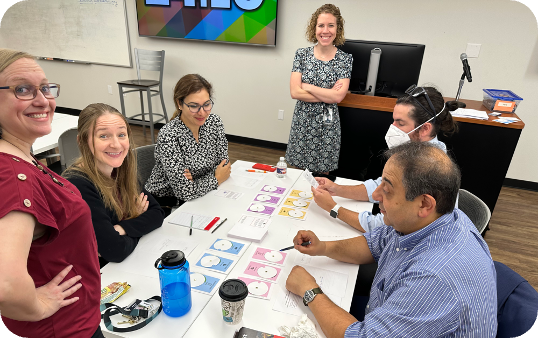
The UNTHSC School of Public Health, in collaboration with the Parker County Hospital District, SaferCare Texas and BEST EMS, is launching an impactful public health video for February's Heart Health Month. The video is part a larger UNTHSC campaign to raise awareness about heart health. The campaign video features real footage of a dramatic rescue…

January 30, 2024
By Sally Crocker Dr. Erika Thompson, associate professor of population and community health at The University of North Texas Health Science Center at Fort Worth School of Public Health, has been elected as secretary for the American Academy of Health Behavior (AAHB). “It is with great pleasure that we announce Dr. Thompson has been elected…

January 26, 2024
By Sally Crocker “Growing up as a Hispanic girl with a single mother in the 1970s and ‘80s when neither was popular or well accepted, I never dreamed that my life would one day have purpose or make an impact on other people’s lives,” Dr. Teresa Wagner recently shared with graduates from the Texas Woman’s…

January 26, 2024
By Sally Crocker Much of Dr Erika Thompson’s work is focused on HPV research and prevention. Recently, she presented a Grand Rounds talk at The University of North Texas Health Science Center at Fort Worth on “Designing, Implementing and Evaluating Interventions to Increase HPV Vaccination across the Life Course.” Thompson is an associate professor of…

January 17, 2024
By Sally Crocker The School of Public Health at The University of North Texas Health Science Center at Fort Worth has released its new strategic plan – IMPACT 2030: Commitment to Community – to steer the course of the school into the future. “The completion of this plan represents months of tireless effort, inclusive collaboration…

Social media