Right resource, right time
By Alex Branch
Dorinda Lopez was trapped in a miserable cycle of sickness.
Weak from spine deterioration and recurrent bacterial skin infections, the 67-year-old woman often fell inside her home at a Fort Worth assisted living center. She constantly dialed 911 for help from firefighters and paramedics, sometimes many times a week.
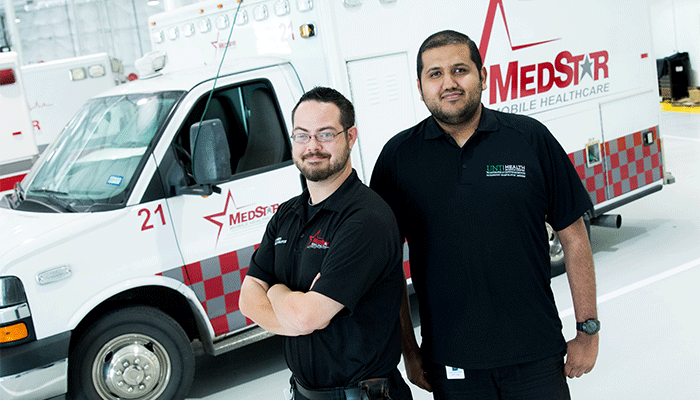
But when certified paramedic John Farris and Osama Sher, then a fourth-year medical student, arrived at her door, their purpose wasn’t to load Lopez into a MedStar ambulance for another trip to the hospital.
In fact, they were there to keep her out of it.
“Dorinda, how are we feeling?” Farris asked, opening a pack of equipment needed to measure blood pressure, draw blood, take an electrocardiogram, access Lopez’ digital health records – or perform many of the other health checks typically done during clinic visits.
“I’m glad to see you,” Lopez answered, under a blanket in her reclining chair. “I was so sick last night, and I was miserable.”
Scheduled house calls stir the nostalgia of small-town doctoring, but Farris and Sher are on the cutting edge of innovation. They’re practicing mobile integrated health care, an innovative health care delivery model that provides value, promotes teamwork and improves outcomes for patients.
This integrated approach to care delivery ensures patients in out-of-hospital settings receive the right resource at the right time, preventing unnecessary emergency department visits and readmissions. Unlike traditionally siloed health care groups, mobile integrated health care brings together clinical specialists who coordinate care across the continuum.
Medical students in UNTHSC’s Texas College of Osteopathic Medicine are the first in the nation to experience clinical training through multidisciplinary rotations centered on mobile integrated health care. The university is partnering with Medstar Mobile Healthcare, which provides emergency ambulance services, and Evolution Health, an integrated medical practice based in Dallas that specializes in the care of complex patients in the home and alternate settings.
For the next hour at Lopez’s apartment, Farris and Sher measured her vital signs, reviewed her diet, translated medical jargon into understandable terms and discussed her medications. They even scoured her kitchen cabinets to make sure the salt substitute she recently bought is safe for her to eat.
“It changes how you think about medicine because you get interaction with the patient that’s impossible in an office or hospital,” Sher said. “I see how she lives, how she eats, whether there is a railing for her to grab for assistance and who she has here to help her.”
Training opportunities are not just for medical students. Because health care is an interprofessional effort, UNTHSC physician assistant students and pharmacy students are participating with health care teams at Evolution and MedStar, said Darrin D’Agostino, DO, Associate Dean of Community Medicine.
“Our students are learning to care for patients on the patient’s terms,” Dr. D’Agostino said. “This is the future.”
Making a difference
Farris and Sher already have seen Lopez’s health improve.
Her calls to 911 have dropped to almost zero since they started visiting her two to three times a week earlier this year. Farris and Sher help her log health information in a black binder that she takes to all her appointments.
During each visit, Lopez, Farris and Sher review the book to make sure she understands all the health providers’ instructions, and that her care is properly coordinated.
“They explain everything so thoroughly,” Lopez said. “Even when I’m sick, I feel better by the time they leave.”
MedStar launched its mobile integrated health program in 2009 to address patients who routinely called 911 for nonemergency purposes. For example, the same 21 patients accounted for more than 2,000 MedStar trips to a hospital emergency room in a single year.
At the same time, the way hospitals are paid for treating patients started shifting. The federal government began giving hospitals financial incentives and enacting penalties to reduce hospital readmissions and emphasize quality of care instead of quantity of care.
MedStar found motivated partners in hospitals such as JPS Health Network, physicians groups, hospices and home health care agencies eager to refer patients like Lopez to the MedStar managed care program.
The program has made an impact, said Vicki Nejtek, PhD, Associate Professor in the Center for Alzheimer’s and Neurodegenerative Disease Research. She received a grant from MedStar to evaluate the success of the mobile integrated health program.
From 2009 to 2015, program participation significantly improved the health of 73 percent of patients who frequently used emergency department services for non-emergency reasons, reducing their emergency department use by an average of 87 percent and saving more than $6 million, according to preliminary results of Dr. Nejtek’s evaluation.
“This is a wonderful opportunity for our medical students to see first-hand how to successfully work with a multidisciplinary team of health professionals to provide integrated levels of care that will greatly benefit the patient while reducing health care system costs,” Dr. Nejtek said.
UNTHSC medical students also contribute clinical expertise to the program, said Matt Zavadsky, public affairs director for MedStar Mobile Healthcare.
“Our mobile health practitioners can learn from the students, too,” Zavadsky said. “Our people and students working side-by-side together with patients is invaluable for both of them.”
Building trust
At Lopez’s apartment, Farris and Sher finish their appointment. They update her black binder and review the medications she is taking to make sure she understands the schedule.
It is Sher’s last day in the program. In a few weeks, he will graduate from UNTHSC and leave for Florida for a residency in family medicine. He’ll take his new skills in mobile integrated health with him.
Packing his equipment, Farris asks Lopez if she has any advice to give Osama.
“Yes, the world needs more of you guys,” she said. “And the No. 1 reason is that you make me feel special. Because I know someone is coming all the way over here just to see about me.
“That may sound trivial, but it’s not. I know you and I trust you. And that makes me want to work hard to make myself be healthier.
“You’re going to be a good doctor,” she said.




Social media