Community Blog-Prostate cancer and African-American men: A call for health equity
November 16, 2017 • community
School of Public Health & Texas Center for Health Disparities
Community Blog
 Two years ago, County Commissioner Roy Brooks underwent surgery to remove prostate cancer. Two years prior to that, his brother died of prostate cancer.
Two years ago, County Commissioner Roy Brooks underwent surgery to remove prostate cancer. Two years prior to that, his brother died of prostate cancer.
When interviewed prior to his surgery, Commissioner Brooks said:
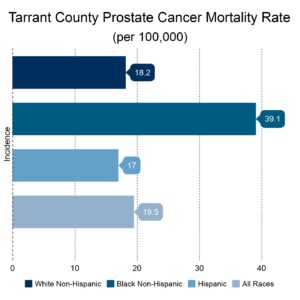
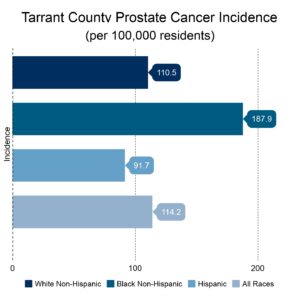
In Tarrant County, the prostate cancer health disparities highlight the higher rate at which African-American men are likely to be diagnosed, receive late stage diagnoses, and to die of prostate cancer, than men of other racial and ethnic groups.
Prostate Cancer Race Disparities in Tarrant County
During the past year, the leadership of the Tarrant County Cancer Disparities Coalition transitioned to Cancer Care Services and their focus expanded from breast cancer to all cancers impacting adults and children in our community. As part of this transition, a county needs assessment was led by Marcela Gutierrez, a faculty member of the University of Texas at Arlington School of Social Work, and board member of Cancer Care Services. Some of their key findings highlighted the large disparities African-Americans endure with prostate, colorectal and breast cancer.
Inequalities versus Inequities
 These local findings are consistent with national studies of cancer risk and mortality where African-American men are twice as likely to die from prostate cancer as men in other racial groups, even after accounting for education and income1. Understanding why these disparities exist is a complex puzzle for researchers and many are making efforts to distinguish between two types of disparities; inequalities include differences based on genetics or other biological factors and inequities are “unjust structural conditions that shape health outcomes”,2 p. 790.
These local findings are consistent with national studies of cancer risk and mortality where African-American men are twice as likely to die from prostate cancer as men in other racial groups, even after accounting for education and income1. Understanding why these disparities exist is a complex puzzle for researchers and many are making efforts to distinguish between two types of disparities; inequalities include differences based on genetics or other biological factors and inequities are “unjust structural conditions that shape health outcomes”,2 p. 790.
Understanding and finding solutions to both are important. Research in the area of personalized medicine is intended to identify better ways of identifying genetic risks, as well as targeting the right kinds of treatment for individual needs. These efforts that focus on inequalities are crucial because a “one size fits all” approach to medicine does not work and could actually cause harm.
Identifying and finding solutions to inequities involves looking at social, behavioral, and environmental factors that influence cancer incidence and survival. We know that certain health behaviors may help prevent prostate cancer, such as eating vegetables3 and engaging in physical activity4. However, current research is showing inequities in access to healthy food5 and neighborhood characteristics that reduce the likelihood of walking or being physically active6,7.
Race may play a role in seeking care and preventive services. One study showed that experiencing racism in health-care settings was associated with a 79% increase of not being up-to-date on prostate cancer screening8. These delays may result in late-stage diagnosis. In Tarrant County, there is a late-stage diagnosis rate disparity of 18.3% for African-American men versus 14.7% for White men.
Other studies point to racial differences in allostatic load, a physical indicator of chronic stress and health decline9, which can add to racial disparities in mortality10. Approximately 17% of the prostate cancer gap in death rates between African-American and White men is associated with differences in physicians and their treatment choices11. For example, active treatment for prostate cancer is more likely to be delayed for African-American men than for White men12.
Tarrant County Cancer Disparities Coalition
Collectively, local and national data point to the need to act. The Tarrant County Cancer Disparities Coalition was launched more than five years ago through support from the Texas Center for Health Disparities, a National Institute of Health Center of Excellence at the University of North Texas Health Science Center. In its new home at Cancer Care Services, the coalition is ready to develop new and innovative partnerships to help reduce or eliminate cancer disparities that affect the lives of cancer patients, caregivers and survivors in Tarrant County. If you are interested in helping, participating in the coalition is a great way to join forces with other community stakeholders and advocate for change. To receive more information about the Coalition, contact Cancer Care Services at 817-921-0653.
Another way to get involved is to attend the 4th annual Prostate Cancer Screening event , led by Commissioner Brooks on February 18, 2018. Partnering with the UT Southwestern Moncrief Cancer Institute, Tarrant County Public Health Department, and JPS; the event will offer both education and screening.
Authors:
Emily Spence-Almaguer, MSW, PhD
Associate Dean for Community Engagement and Health Equity
Associate Professor, School of Public Health
Community Engagement Core Director, Texas Center for Health Disparities
University of North Texas Health Science Center
Marcela Gutierrez, LMSW
Assistant Professor in Practice, School of Social Work
Faculty Research Associate, Center for Mexican American Studies
University of Texas at Arlington
Teresa Wagner, DrPH, RDN, CPH
Assistant Professor, School of Public Health
University of North Texas Health Science Center
Katherine Cantu Anguiano, MPH, CPH
Project Coordinator, School of Public Health
University of North Texas Health Science Center
Special thanks to Betty Tonui for her work in collecting statistical information about cancer disparities inTarrant County.
References
- Singh, G.K., & Jemal, A. (2017) Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States 1950-2014: Over six decades of changing patterns and widening inequalities. Journal of Environmental and Public Health, https://doi.org/10.1155/2017/2819372
- Wailoo, K. (2017). Cancer and race: What they tell us about the emerging focus of health equity. Journal of Health Politics, Policy and Law, 42 (5), doi: 10.1215/03616878-3940441.
- Cohen, J.H., Kristal, A.R., Stanford, J.L. (2000) Fruit and vegetable intakes and prostate cancer risk. J Natl Cancer Inst, 5(92): 61-68. American Journal of Public Health, 96 (5): 826-833.
- Clarke, G. & Whittemore, A.S. (2000). Prostate cancer risk in relation to anthropometry and physical activity: The National Health and Nutrition Examination Survey epidemiological follow-up study. Cancer Epidemiology, Biomarkers & Prevention, 9(9): 875-881.
- Larson, N.I., Story, M.T., & Nelson, M.C. (2009) Neighborhood environments: Disparities in access to healthy foods in the US. Am J Prev Med, 36(1): 74-82.
- Addy, C.L., Wilson, D.K., Kirtland, K.A., Ainsworth, B.E., Sharpe, P., & Kimsey, D. (2004). Associations of perceived social and physical environmental supports with physical activity and walking behavior. American Journal of Public Health, 94 (3): 440-444.
- Franzini, L., Taylor, W., Elliot, M.N., Cuccaro, P., Tortolero, S.R., Gilliland, J., & Schuster, M. (2010). Neighborhood characteristics favorable to outdoor physical activity: Disparities by socioeconomic and racial/ethnic composition. Health and Place, 16: 267-274.
- Shariff-Marco, S., Klassen, A.C., & Bowie, J.V. (2010). Race and ethnic differences in self-reported racisim and its association with cancer-related health behaviors. American Journal of Public Health, 100: 364-374. doi: 10.2105/AJPH.2009.163899.
- Geronimus, A.T., Hicken, M., Keen, D. & Bound, J. (2006) “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States.
- . Duru, O.K., Harawa, N.T., Kermah, D., & Norris, K.C. (2012). Allostatic load burden and racial disparities mortality. J Natl Med Assoc. 104 (1-2), 89-95.
- Taskler, G., Keating, N.L., & Cutler, D.M. (2012) Explaining racial differences in prostate cancer mortality. Cancer, doi: 10.1002/cncr.27379.
- Shavers, V.L., Brown, M., Klabunde, C.N., Potosky, A.L. Davis, W.D., Moul, J. & Fahey, A. (2004). Race/ethnicity and the intensity of medicial monitoring under ‘watchful waiting’ for prostate cancer. Medical Care, 42(3): 239-250.
Research reported in this publication was supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number U54MD006882. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.

Social media