School of Public Health
Month: September 2020

September 30, 2020 • Uncategorized
September 23, 2020 • Uncategorized
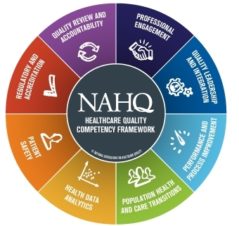
Master of Health Administration students will prepare to achieve Certified Professional in Healthcare Quality® certification during capstone course. The HSC School of Public Health has collaborated with the National Association for Healthcare Quality (NAHQ) to provide its Master of Health Administration (MHA) students with the opportunity to pursue the only accredited certification in healthcare quality, the…

September 21, 2020 • Uncategorized
By Sally Crocker HSC 2020 graduate Julia Aiken was finishing the last semester of her MPH in Public Health Practice when COVID-19 hit this spring. By May, she had wrapped up her degree and was helping out with Tarrant County Public Health’s (TCPH) contact tracing efforts, to track and help stop community spread of the…

September 15, 2020 • Uncategorized
By Sally Crocker Health inequality and systemic racism have long threatened the lives of African Americans. The COVID-19 pandemic and increased awareness of police violence in 2020 have intensified nationwide action toward solutions and change for traditionally underserved populations. For health disparities researchers like HSC Assistant Professor Erica Spears, PhD, who has dedicated her…

Social media