Caroline Rickards
Caroline Rickards, Ph.D.
Associate Professor
Physiology
caroline.rickards@unthsc.edu
Education
- PhD, RMIT University, (Melbourne, Australia (2005)
Curriculum Vitae
UNTHSC Experts https://experts.unthsc.edu/en/persons/caroline-rickards https://scholar.google.com/citations?hl=en&user=7w9W8pkAAAAJ
Lab Facebook (https://www.facebook.com/Cerebral-and-Cardiovascular-Physiology-Laboratory-517797054950112)
Cerebral Blood Flow Virtual Seminar Series ( http://www.car-net.org/content/resources#tabSeminars)
Personal Bio
Dr. Caroline Rickards received her PhD from RMIT University in Melbourne, Australia in 2005. She was a postdoctoral fellow at the US Army Institute for Surgical Research, and a Research Assistant Professor at the University of Texas at San Antonio before joining UNTHSC in 2012. In addition to her active research program, Dr. Rickards teaches cardiovascular physiology to medical and graduate students, including the Master’s in Medical Sciences and traditional PhD/MS programs. Dr. Rickards is an active member of the local UNTHSC community, most notably as Vice Chair of the IRB, Senator on the Faculty Senate, and founding member of the Women Faculty Network. Outside of UNTHSC, Dr. Rickards serves on the editorial boards of the Journal of Physiology, and the American Journal of Physiology- Regulatory, Integrative and Comparative Physiology, she is Secretary of the Cerebral Autoregulation Research Network (CARNet), an Environmental Physiology Councillor for the Exercise & Environmental Physiology Section of the American Physiological Society, and she was Chair of the American Physiological Society Women in Physiology Committee (2015-2017). In her spare time, Dr. Rickards enjoys spending time with her family (including 2 rescue dogs), hitting the hiking trails, and exploring new places around the world (4 continents, and 30 US states so far).
Research Interests
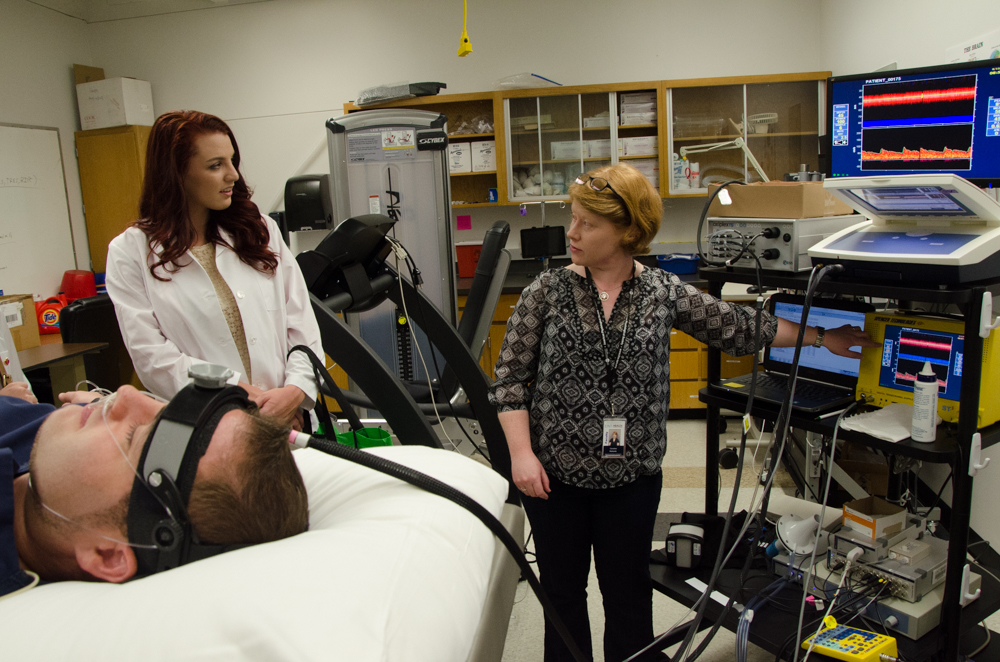
The general research interests of the Cerebral & Cardiovascular Physiology Laboratory encompass understanding vital organ perfusion in humans under stress. The laboratory is specifically focused on the regulation of brain blood flow and oxygenation during stressors that challenge cerebral perfusion such as traumatic hemorrhage, cardiac arrest, and stroke. A major research focus has been on the early detection of hemorrhagic injury in trauma patients, characterizing physiological differences between individuals with high versus low tolerance to this stress. In addition to investigating these physiological mechanisms, we also collaborate with academic, industry, and government partners to develop and test sensor technologies that may improve the early detection of tissue hypoperfusion in clinical settings. We also study potential therapies that may improve cardiovascular and cerebrovascular tolerance to hypoperfusion, including resistance breathing, oscillatory perfusion therapy, and occlusive exercise.
Research Keywords
Cerebral blood flow; cerebral tissue oxygenation; hemorrhage; lower body negative pressure
Current Projects
- Pulsatile Perfusion Therapy Phase II: A novel approach for improving cerebral tissue blood flow and oxygenation (American Heart Association, Grant-in-Aid)
- Pulsatile Perfusion Therapy Phase III: Sympathetic activity and neurovascular transduction (American Heart Association, Transformational Project Award)
Current Funding
- Rickards (PI), Yurvati (Co-I), American Heart Association (AHA) Association Transformational Project Award (19TPA34910073). “Phase II: A novel approach for improving cerebral tissue blood flow and oxygenation via pulsatile perfusion therapy” (07/19 – 06/22)
- Rickards (PI), Yurvati (Co-I), American Heart Association (AHA) Association Wide Grant-in-Aid (17GRNT33671110). “A novel approach for improving cerebral tissue blood flow and oxygenation via pulsatile perfusion therapy” (07/17 – 03/21, NCE)
- Anderson (PI), Rickards (Mentor), American Heart Association (AHA) Predoctoral Fellowship (20PRE35210249). “Hemodynamic Oscillations and Protection of Cerebral Tissue Oxygenation” (05/20 – 4/22)
Selected Publications
- Hansen A, Lawley J, Rickards CA, Howden E, Sarma S, Cornwell III W, Amin S, Mugele H, Marume K, Possnig C, Whitworth L, Williams M, Levine BD. Reducing Intracranial Pressure by Reducing Central Venous Pressure: Assessment of potential countermeasures to spaceflight associated neuro-ocular syndrome. J Appl Physiol 2020 (In Press).
- Rosenberg AJ*, Kay VL*, Anderson GK*, Sprick JD*, Rickards CA. A Comparison of Protocols for Simulating Hemorrhage in Humans: Step vs. Ramp Lower Body Negative Pressure. J Appl Physiol 2020 (In Press).
- Anderson GK*, Sprick JD*, Park FS*, Rosenberg AJ*, Rickards CA. Responses of cerebral blood flow and tissue oxygenation to low frequency oscillations during simulated hemorrhagic stress in humans. Exp Physiol 2019; 104:1190-1201 (PMID 31090115).
- Rickards CA. Vive la résistance! The Role of Inspiratory Resistance Breathing on Cerebral Blood Flow. Resp Physiol & Neurobiol 2019; 265: 76-82. (PMID 30340016)
- Park FS*, Kay VL*, Sprick JD*, Rosenberg AJ*, Anderson GK*, Mallet RT, Rickards CA. Oxidative stress response during stimulated hemorrhage via application of lower body negative pressure. Exp Biol Med 2019; 244: 272-278 (PMID 30727766).
- Sprick JD*, Przyklenk K, Mallet RT, Rickards CA. Ischemic and hypoxic conditioning: Potential for protection of vital organs. Exp Physiol 2019; 104(3): 278-294. (PMID 30597638) Crandall CG, Rickards CA, Johnson BD. Impact of Environmental Stressors on Tolerance to Hemorrhage in Humans. Am J Physiol Regul Integr Comp Physiol 2019; 316: R88-R100. (PMID 30517019) Sprick JD*, Rickards CA. Cyclical Blood Flow Restriction Resistance Exercise: A Potential Parallel to Remote Ischemic Preconditioning? Am J Physiol Regul Integr Comp Physiol 2017; 313:R507-R517 (PMID 28835448; DOI: 10.1152/ajpregu.00112.2017)
- Sprick JD*, Rickards CA. Combining Remote Ischemic Preconditioning and Aerobic Exercise: A Novel Adaptation of Blood Flow Restriction Exercise. Am J Physiol Regul Integr Comp Physiol 2017; 313:R497-R506 (PMID 28835447; doi: 10.1152/ajpregu.00111.2017)
- Kay VL*, Sprick JD*, Rickards CA. Cerebral Oxygenation and Regional Cerebral Perfusion Responses with Resistance Breathing during Central Hypovolemia. Am J Physiol Regul Integr Comp Physiol 2017; 313:R132-R139 (PMID 28539354; DOI: 10.1152/ajpregu.00385.201)
- Kay VL*, Rickards CA. The role of cerebral oxygenation and regional cerebral blood flow on tolerance to central hypovolemia. Am J Physiol Regul Integr Comp Physiol 2016; 310(4): R375-83 (PMID 26676249)
- Rickards CA, Johnson BD, Convertino VA, Joyner MJ, Barnes JN. Cerebral blood flow regulation during blood loss compared to lower body negative pressure in humans. J Appl Physiol 2015; 119(6): 677-85.
- Rickards CA. Cerebral blood flow regulation during hemorrhage. Compr Physiol 2015; 5: 1585-1621. Rickards CA, Tzeng YC. Arterial pressure and cerebral blood flow variability: friend or foe? A review. Front Physiol 2014; 5:120.
- Ryan KL, Rickards CA, Hinojosa-Laborde C, Cooke WH, Convertino VA. Arterial pressure oscillations are not associated with muscle sympathetic nerve activity in individuals exposed to central hypovolemia. J Physiol 2011; 589:5311-5322.
- Rickards CA, Ryan KL, Cooke WH, Convertino VA. Tolerance to central hypovolemia: the influence of oscillations in arterial pressure and cerebral blood velocity. J Appl Physiol 2011; 111: 1048-1058.
- Rickards CA, Ryan KL, Ludwig DA, Convertino VA. Is heart period variability associated with the administration of life saving interventions in individual, pre-hospital trauma patients with normal standard vital signs? Crit Care Med 2010; 38(8):1666-73.
- Cooke WH, Rickards CA, Ryan KL, Convertino VA. Muscle sympathetic nerve activity during intense lower body negative pressure to presyncope in humans. J Physiol 2009; 587:4987-4999.
- Convertino VA, Ryan KL, Rickards CA, Salinas J, McManus JG, Cooke WH, Holcomb JB. Physiological and medical monitoring for en route care of combat casualties. J Trauma 2008; 64: S342-53.
- Rickards CA, Ryan KL, Cooke WH, Lurie KG, Convertino VA. Inspiratory resistance delays the reporting of symptoms with central hypovolemia: association with cerebral blood flow. Am J Physiol Regul Integr Comp Physiol 2007; 293:R243-R250.
Teaching Interests
- Cardiovascular Physiology
- Physiology Journal Club
UNTHSC Committees and Service
- Founding Member & Chair, Women Faculty Network (WFN)
- Senator, Faculty Senate GSBS DE&I Working Group Vice Chair, IRB
National Committees and Service
- Co-Organizer, Cerebral Blood Flow Virtual Seminar Series
- Committee on Committees, Exercise & Environmental Physiology Section Representative, American Physiological Society
- Environmental Physiology Councillor (Elected)
- Exercise & Environmental Physiology Section, American Physiological Society Secretary (Elected)
- Cerebral Autoregulation Research Network (CARNet)
- Reviewing Editor, Journal of Physiology Editorial Board, American Journal of Physiology-Regulatory, Integrative and Comparative Physiology

Social media