Mountain highs
By Sarah Hewitt
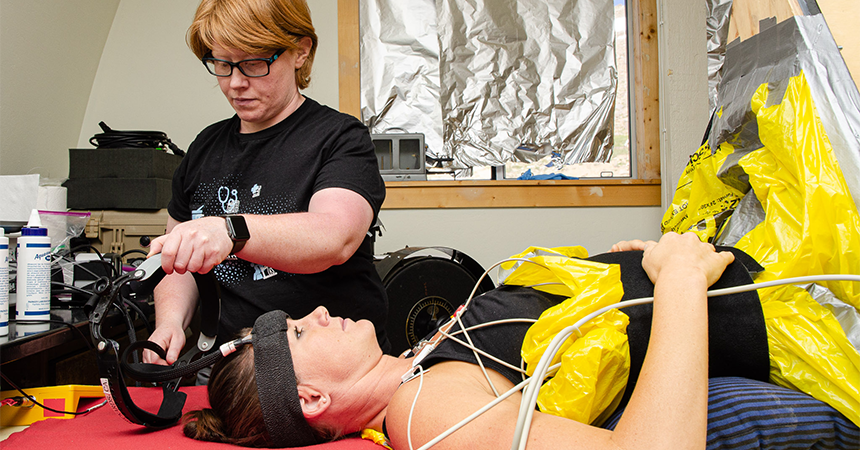
I lay on my back on a table with my lower body from the waist down inside a triangular wooden box, not unlike a magician’s box as if I’d volunteered to be sawed in half. Dr. Caroline Rickards, an associate professor from UNT Health Science Center at Fort Worth, secured a neoprene belt across my abdomen, then tucked plastic bags around me to form an airtight seal between my lower body in the box and my upper body on the table. Hoses attached two industrial-strength vacuum cleaners to the box so that when they were turned on, they produced a suction pressure to anything inside – in this case, half of me.
Dr. Rickards is an expert in using a technique called lower body negative pressure (LBNP). For almost 20 years, she’s used LBNP as a tool to simulate blood loss to better understand how the body responds when the brain is deprived of oxygen. She’s studied fighter pilots in high G forces and helped develop treatments for soldiers in the U.S. Army who suffered blood-loss injuries. But she’s always had an interest in high-altitude physiology and how the lack of oxygen at altitude can change the body’s response to simulated hemorrhage. Last August, she had a chance to find out.
Dr. Rickards and two members of her lab, Dr. A.J. Rosenberg, a postdoctoral fellow, and Garen Anderson, a doctoral student, joined a team of 25 people from six universities in Canada, Ireland and the U.S. at Barcroft Research Station. The station sits at the end of a hazardous mountain road, 12,500 feet up the slopes of White Mountain in the California Sierras, and we spent 12 days collecting data for 12 distinct studies on the effects of high altitude on human physiology. I’d volunteered to be a guinea pig.
Testing equipment
At altitudes above 10,000 feet, hypoxia (the lack of oxygen) can trigger symptoms of acute mountain sickness – breathlessness, headache, nausea, dizziness, confusion and sleep apnea. Within hours of arriving at Barcroft, we were all experiencing symptoms to some degree.
The station, built in 1951, has three lab spaces and a full workshop, which is handy since there’s nowhere to go for replacement parts. That evening, as people’s symptoms set in, the labs were set up and equipment was tested so experiments could start right away.
“Those first couple days, I was not feeling very well,” Dr. Rosenberg said, “I had real bad headaches and was having a hard time sleeping.”
For 12 days, 25 people spent 24/7 together, shared two bathrooms and with the exception of a couple of rest days, ran experiments 10-12 hours a day. A schedule, pinned to the wall in the kitchen, carefully orchestrated the shuffling of researchers from one lab to be slotted in as participants in another, ensuring that everyone could make their quota of experiments.
We started referring to people by the university from which they hailed, all except for Rickards’ group – they became simply Team Texas, and it was quickly evident that everyone could use a little Team Texas in their labs. Dr. Rickards, Dr. Rosenberg, and Anderson were constantly assisting with protocols in other labs or acting as participants, pitching in wherever they were needed. But they were focused and ready when their own experimental time slot came up.
“We’re happy back home to do three experiments in a week,” Dr. Rickards said. But there, her team had to squeeze 16 experiments into three days.
“We’re interested in examining the physiological responses to blood-loss injuries and other conditions where you have reductions in brain blood flow like stroke or cardiac arrest,” she said. “But the other part is developing therapeutic interventions that might improve the responsiveness to a blood-loss injury – to see if we can improve long-term survival.”
Far-reaching applications
And there are far-reaching applications to their work.
“We have soldiers who are fighting in high-altitude environments,” Dr. Rickards said. “But it also could benefit individuals who have bleeding injuries at altitude like hikers, mountaineers, people on snowmobiles who have massive accidents – it’s got applications to both the military and civilian setting.”
They’ve termed one of their interventions “pulsatile perfusion therapy,” in which they oscillate the blood pressure and blood flow in waves to try and improve tissue perfusion.
“If people respond better with the waves,” Anderson said, “we could move that into a clinical setting where people are being treated using that model.”
Each participant is tested in two conditions, one where they simulate blood loss with oscillations, and one without that pushes people to their maximal tolerance. I was being prepped for the max tolerance test.
This wasn’t the first time LBNP has been used at altitude, but it was the first time anyone had tried maximal tests. The suction in the box is gradually turned up to draw increasingly more blood away from the brain, reducing brain blood flow by 30% to 40%. The protocol continues until the subject calls it quits or until their systolic blood pressure drops below a predetermined cut-off point.
Physiological stress
“It’s a really big physiological stress,” Dr. Rickards admitted, “and when you throw in hypoxia on top of that, I wasn’t sure how people were going to respond.”
She attached the ECG leads to the 12 electrodes stuck to my chest, and Dr. Rosenberg confirmed that my heart rate was showing on the monitor. He then attached a blood pressure cuff around my right arm and fit a pulse oximeter on my middle finger to track my blood pressure and oxygen saturation, while Anderson inserted a nasal cannula. He then slipped a plastic headband on my forehead, screwed it into place, and started to position the Doppler ultrasound probes that would monitor my brain blood flow.
The brain is a greedy organ. It needs a constant supply of blood to continue functioning so a significant drop in pressure can lead to a loss of consciousness, brain damage or death. LBNP is a useful technique to safely mimic this in a laboratory setting, and Dr. Rickards has plenty of experience.
She received her PhD in aerospace physiology in her native Melbourne, Australia, after using the LBNP technique as a training method to improve cardiovascular responsiveness in pilots from the Royal Australian Air Force. She then started a postdoctoral fellowship with the U.S. Army Institute for Surgical Research in San Antonio, Texas. There she helped develop technologies to better detect blood loss from internal injuries and to measure how a patient responds to treatment.
Different pace
Dr. Rickards spent seven years in San Antonio before moving back into academia at HSC. “In that military environment, there’s an urgent need for treatment because soldiers are dying on the battlefield,” she said. “But the pace is a little different in the academic environment where we’re also trying to develop therapies and interventions that might improve human health, but with a longer-term view.”
Dr. Rickards checked with me to see if I was ready.
“Stay nice and still and relaxed for us, let us know if you feel any symptoms and want us to stop.”
After five quiet minutes collecting my baseline data, I saw Anderson give a nod to Dr. Rickards, and she flipped the switch. The vacuums roared to life. The sudden suction dragged me a few inches along the table, drawing me into the box. I shifted position slightly, remembered to relax my lower body, and focused on the ticking metronome to regulate my breath.
Most people make it to stage two or three. Stage one passed, and then stage two, and I felt confident that I could handle it. At stage three, I started to count my breaths, estimating that 50 breaths should be about five minutes. And 52 breaths later, they turned it up again to the fourth and final stage.
Now the vacuums drowned out other noises and the intense suction of the neoprene sleeve around my waist made it increasingly strenuous to breathe. I tried to will my body to adjust – determined that if I could make it this far, I could handle the rest.
“I feel good,” I told myself on one shaky breath. “I can do it.” And then suddenly, I couldn’t. My vision closed in, and I knew I couldn’t stabilize. At precisely that moment, Dr. Rickards, Anderson and Dr. Rosenberg simultaneously yelled, “Stop!” and the vacuum mercifully shut off. Instantly, I felt a rush of blood surging back to my heart, lungs, and brain that were yearning for it.
Withstand the test
“Wowza, you’re a beast!” Dr. Rickards exclaimed. “I thought you were going to max out our protocol!” I laughed with relief and a misplaced sense of pride at lasting so long. In truth, it was out of my control, and what makes one person able to withstand the test while another blacks out in the first few minutes still is not understood.
“We thought hypoxia would make things a little bit harder on people, but it’s kind of a mixed bag of responses,” Anderson said.
“Some people are more tolerant, some people are less tolerant,” Dr. Rickards agreed. “And that in itself it quite interesting.”
But they each cautioned against brash conclusions. “We have to look at the data more thoroughly and do some analysis,” Dr. Rosenberg reminded me, “so it’s still TBA!”
Day 8 was the only day the entire team had off together, and most people chose to trek to the peak of White Mountain, which at 14,252 feet is the third highest in California. We slowly zig-zagged up steep switchbacks, past a herd of grazing mountain sheep, and finally reached the peak. We looked out over Owens Valley, about 10,000 vertical feet below, and the Sierra Nevadas rising up on the other side.
“It’s been 20 years in the making that I’ve been wanting to do a high-altitude expedition,” Dr. Rickards reflected. I asked her how she thought it went and without a second’s hesitation, she laughed and said, “We knocked out 16 experiments in two and a half days! I didn’t know if it would be possible, and we’ve discovered that it is. It’s just shown us what we’re capable of.”
On our last night at Barcroft, everyone gathered upstairs, crammed onto three couches or lying on the floor. After years of planning and overcoming logistical hurdles, each team had pulled off every experiment they’d proposed, and the sense of accomplishment, and relief, was palpable.
While all the teams performed admirably, “well-oiled machine,” “expert” and “professional” were just some of ways people described the Rickards’ group. So during the awards ceremony we held that night, one award was no surprise, the Top Team award, the only serious award of the bunch. And there was only one team in the running – Team Texas.
Dr. Sarah Hewitt is a biology professor at Mount Royal University in Calgary, Canada, and an adventure scientist who travels all over the world to work with scientists in the field and then writes about it.




![Uyen Sa Nguyen Scaled[58]](https://www.unthsc.edu/newsroom/wp-content/uploads/sites/16/Uyen-Sa-Nguyen-scaled58-145x175.jpg)

Social media