Research opens new doors to treating glaucoma
By Jan Jarvis
Glucocorticoids are often used to reduce inflammation, reduce pain and treat many conditions such as allergies and rashes. But for some people, the very drugs that treats one condition can cause another: specifically, glaucoma.
The condition, which affects more than 64.3 million people, is the second-leading cause of irreversible blindness in the world. Still, little is known about why glucocorticoid therapy elevates intraocular pressure and raises the risk of developing this disease, said Gulab Zode, PhD, Assistant Professor in Pharmacology & Neuroscience.
“We know that when people are treated with glucocorticoids, one of the possible side effects is increased intraocular pressure,” he said. “About 30 percent to 40 percent of patients develop this and if they don’t get treated, they experience vision loss.”
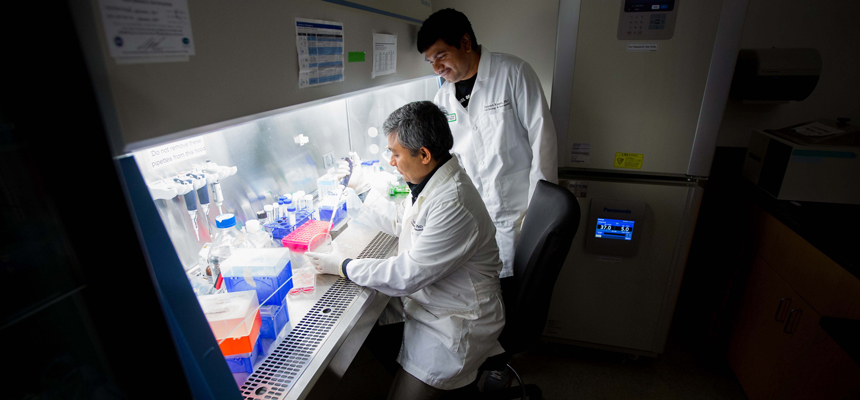
In a paper recently published in the Journal of Biological Chemistry, a team of scientists led by Dr. Zode discovered how glucocorticoids elevate intraocular pressure in the eye.
“There are no treatments that target the pathology of this disease, there are only drugs that act on the symptoms,” he said, “I want to know what causes the damage so that a targeted treatment could be developed.”
For years, Dr. Zode’s research has focused on what causes damage to the trabecular meshwork, a specialized tissue in the eye that maintains normal intraocular pressure by regulating aqueous humor outflow resistance.
In this article, Dr. Zode’s lab identified that glucocorticoids increase the transforming growth factor B2, which further contributes to elevation of intraocular pressure. The study establishes a central role for transforming growth factor B2 in glucocorticoid-induced glaucoma and provides therapeutic targets for the reduction of increased intraocular pressure in the eye.
“Now that we can see how transforming growth factor B2 plays a role in intraocular pressure elevation, we can block this signaling pathway,” he said. “This opens the door to the possibility of targeted treatment.”


![Uyen Sa Nguyen Scaled[58]](https://www.unthsc.edu/newsroom/wp-content/uploads/sites/16/Uyen-Sa-Nguyen-scaled58-145x175.jpg)


Social media